
2024/12/11
Breastfeeding confers immuno-protective factors to the baby and helps build the baby’s own lifelong immune system.
Breastfeeding is now more important than ever as optimal nutrition for the child on the one hand, and on the other hand because of its important role for the human immune system for lifelong health.
IBFAN document: Breastfeeding and the immune system
Document published by IBFAN with 25 scientific references (Carol Bartle et al. 2023)
The immune system of the newborn
The immune system of tne newborn is immature at birth. Breastfeeding not only protects the child through the transfer of immunoglobulins and other immunocompetent factors, but breastmilk helps the baby to strengthen and mature his or her immune system.
As researcher Lars A. Hanson wrote as early as 2004: Breastfeeding protects the baby, and in addition, it nourishes him. Major components of human milk are not primarily for nutrition, but for host defense (see Immunobiology of Human Milk – How Breastfeeding protects babies, 2004) .
Knowledge and research into the dynamic, protective and physiological-immune role of breast milk reveal its important role and lasting impact on the health of the breastfed child – the health of the future adult.

Microbiota
The microbiota is the wide variety of microorganisms that live in a certain environment: so the “human microbiota” includes all bacteria, viruses, fungi, and other single-celled organisms living in the human body. Every human body is host to anywhere between 10 trillion and 100 trillion microorganisms from over 1,000 different species. These organisms live in many different sites of the human body, such as skin, gut, mouth, lungs, and more like in breastmilk.
Breastfeeding builds and nourishes the child’s microbiota, and breast milk acts on the intestinal flora and mucous membranes, two important protective filters against pathogens and viruses. As researcher Lars A Hanson wrote as early as 2004: breastfeeding not only protects the baby, but also nourishes it: “The main components of human milk are not primarily for feeding, but for defending the baby. (in Immunobiology of Human Milk – How Breastfeeding protects babies, 2004).
Microbiota and immune system
Ames et al. (2023) describe the broad impact of breastfeeding on the microbiota and the development of the immune system. The immune system is immature at birth. Active B and C lymphocytes can be detected in children from 12 weeks onwards, but they are much more likely to induce tolerance to antigens than to participate in the fight against pathogens. In addition, the intestinal barrier is somewhat permeable for at least the first 6 months, allowing the translocation of macromolecules such as immunoglobulins (Ig).
The intestinal microbiota is established during the first few weeks, and will have a major impact on the development of the immune system, including the acquisition of oral tolerance and the establishment of defences against pathogens. A good understanding of all the factors, particularly dietary factors, that modulate all these phenomena is essential if we are to optimise them in all infants. The authors provide an overview of the subject: immune cells, enzymes and bioactive proteins, immunoglobulins, oligosaccharides, miRNA, etc. Above all, they note that: “Industrial milks contain almost none of the immunomodulating components of human milk, and they do not provide a dynamic, personalised nutritional intake.” https://pubmed.ncbi.nlm.nih.gov/37055920/
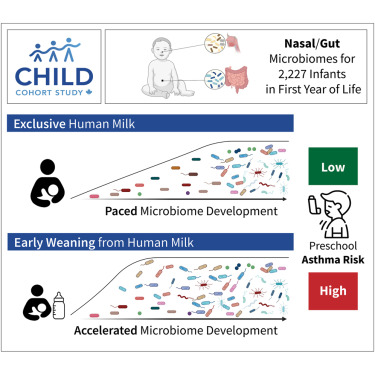
Nasal and gut microbiom
Breastfeeding and microbial colonization during infancy occur within a critical time window for development, and both are thought to influence the risk of respiratory illness. However, the mechanisms underlying the protective effects of breastfeeding and the regulation of microbial colonization are poorly understood. Here, we profiled the nasal and gut microbiomes, breastfeeding characteristics, and maternal milk composition of 2,227 children from the CHILD Cohort Study. We identified robust colonization patterns that, together with milk components, predict preschool asthma and mediate the protective effects of breastfeeding. We found that early cessation of breastfeeding (before 3 months) leads to the premature acquisition of microbial species and functions, including Ruminococcus gnavus and tryptophan biosynthesis, which were previously linked to immune modulation and asthma. Conversely, longer exclusive breastfeeding supports a paced microbial development, protecting against asthma. These findings underscore the importance of extended breastfeeding for respiratory health and highlight potential microbial targets for intervention. Shenhav et al. 2024 https://www.cell.com/cell/fulltext/S0092-8674(24)00782-7
Thymus
During the first two years of life, the thymus gland of the breastfed child is exceptionally large. It is the “organ” that produces T-lymphocytes or “killer” lymphocytes of infected cells and therefore plays an important role in the fight against immune aggression. In the non-breastfed child, the thymus is only half the size.
HAMLET
The protein-lipid complex HAMLET (human alpha-lactalbumin made lethal to tumor cells) has a broad spectrum of activity against cancer cells of different origin. (Ho et al. 2017 https://www.sciencedirect.com/science/article/abs/pii/S0006291X1631779X)
Antiviral properties
The act of breastfeeding means more than just the nutritious transfer of human milk. It is a dynamic biological process that requires close contact between mother and baby so that the mother produces protective factors via her breast tissue in response to her environment and her own exposure to infectious agents.
- Morniroli D et al. The antiviral properties of human milk: a multitude of defence tools from mother nature. Nutrients 2021; 13: 694. https://www.mdpi.com/2072-6643/13/2/694
- Wedekind SIS, Shenker NS. Antiviral properties of human milk. Microorganisms 2021; 9: 715. https://www.mdpi.com/2076-2607/9/4/715
Breastfeeding confers antibodies against SARS-CoV-2 virus, see the list below.
Immunoprotective factors
The following list shows immuno-protective factors that are transmittetd to the infant via breastfeeding
alpha-Lactalbumin (variant)
alpha-lactoglobulin
alpha2-macroglobulin (like)
ß-defensin-1
Bifidobacterium bifidum
Carbohydrate
Casein
CCL28 (CC-chemokine)
Chondroitin sulphate (-like)
Complement C1-C9
Folate
Free secretory component
Fucosylated oligosaccharides
Gangliosides GM1-3, GD1a, GT1b, GQ1b
Glycolipid Gb3, Gb
Glycopeptides
Glycoproteins (mannosylated)
Glycoproteins (receptor-like)
Glycoproteins (sialic acid-containing or terminal galactose)
Haemagglutinin inhibitors
Heparin
IgA secretory
IgG
IgM
IgD
kappa-Casein
Lactadherin (mucin-associated glycoprotein)
lactoferrin
Lactoperoxidase Lewis antigens
Lipids
Lysozyme
Milk cells (macrophages, neutrophils, B & T lymphocytes)
Mucin (muc-1; milk fat globulin membrane)
Nonimmunoglobulin macromolecules (milk fat, proteins)
Oligosaccharides (about 200 human oligosaccharides are known today)
Phosphatidylethanolamine
(Tri to penta) phosphorylated beta-casein
Prostaglandins E1, E2, F2 alpha
RANTES (CC-chemokine)
Ribonuclease
Secretory IgA (see above, too)
Secretory leukocyte protease inhibitor (antileukocyte protease; SLPI)
Sialic acid-glycoproteins
sialylated oligosaccharides
Sialyllactose
Sialyloligosaccharides on sIgA(Fc)
Soluble bacterial pattern recognition receptor CD14
Soluble intracellular adhesion molecule 1 (ICAM-1)
Soluble vascular cell adhesion molecule 1 (VCAM-1)
Sulphatide (sulphogalactosylceramide)
Trypsin inhibitor
Vitamin A
vitamin B12
Xanthine oxidase (with added hypoxanthine)
Zinc
Covid-19, breastfeeding and the immune protection
Check out our specific page on Covid-19 and breastfeeding
Breastmilk Composition
What’s in Breastmilk – Poster
The list of immunocompetent factors transmitted from mother to child through breastfeeding is not only considerable in itself but reveals part of the way in which breastfeeding functions: it is not a static assembly of ingredients, but a biological liquid resulting from its continuous and dynamic production during breastfeeding and mother-child skin-to-skin contact.
In other words, the fine-tuned adaptation of breast milk is the result of an ongoing dialogue between the mother’s microbial environment and that of her child. Thus, in addition to the many non-specific immunological factors transmitted to the infant, the mother provides targeted anti-infective agents and immunological factors for her child.
Changes in Human Milk during prolonged lactation
The results of a study by Sinkiewicz-Darol E et al (2021) suggest an adaptive role of human milk to the nutritional needs of newborns and older children. This may support the promotion of long-term breastfeeding, including co-breastfeeding. Tandem Breastfeeding: A Descriptive Analysis of the Nutritional Value of Milk When Feeding a Younger and Older Child https://pubmed.ncbi.nlm.nih.gov/33478010/
Human milk after the 2nd year of lactation contains significantly higher concentrations of protein, SIgA, and IgG. High concentration of immunoglobulins and protein during prolonged lactation is an additional argument to support breastfeeding even after introducing solid foods and should be one of the overarching goals in the protection of children’s health. Therefore, it is important to consider when making recommendations that not even the number of feeds per day but breastfeeding, in general, should be continued for as long as possible that the mother and the baby wish to as supplement and support for the maturing immune system of the baby. Czosnykowska-Łukacka MO et al.(2020) https://doi.org/10.3389/fped.2020.00428
Lactoferrin in breastmilk. The concentration of Lf in human milk is lactation-stage related; colostrum contains more than 5 g/L, which then significantly decreases to 2-3 g/L in mature milk. The milk of mothers who are breastfeeding for more than one year is of a standard value, containing macronutrients in a composition similar to that of human milk at later stages. The aim of this study was to evaluate lactoferrin concentration in prolonged lactation from the first to the 48th month postpartum. The mean value of lactoferrin concentration was the lowest in the group of 1-12 months of lactation (3.39 ± 1.43 g/L), significantly increasing in the 13-18 months group (5.55 ± 4.00 g/L; p < 0.006), and remaining at a comparable level in the groups of 19-24 month and over 24 months (5.02 ± 2.97 and 4.90 ± 3.18 g/L, respectively). Czosnykowska-Łukacka MO et al.(2019) https://pubmed.ncbi.nlm.nih.gov/31581741/
Protein content of human milk is negatively associated to volume of milk production, so the decrease in the milk volume predicted an increase in protein content. While the nutritional content of human milk is variable, on average the milk protein concentration during the later stages of lactation is sensitive to the declining output of milk. Studies dating back several decades have shown an increase in the proportion of immunoglobulins, lactoferrin, and serum albumin during weaning or prolonged breastfeeding. Verd S et al. (2018) https://www.mdpi.com/2072-6643/10/8/1124
The aim of another study was to describe longitudinal changes in human milk macronutrient concentrations during the prolonged lactation of healthy mothers from the 1st to the 48th month. For the macronutrient content of milk of mothers breastfeeding for longer than 18 months, fat and protein increased and carbohydrates decreased significantly, compared with milk expressed by women breastfeeding up to 12 months. Moreover, the concentration of fat, protein and carbohydrates in HM over 2 years of lactation from the 24th to the 48th month remained at a stable level. Czosnykowska-Łukacka MO et al.(2018) https://pubmed.ncbi.nlm.nih.gov/30513944/
Difference between breastfeeding and feeding with human milk
There is a significant difference between
- breastfeeding with skin to skin contact and transfer of the mother’s antibodies and the anti-infective agents in the live cells to her child, and
- the feeding with human milk using expressed (and transformed) breastmilk and delivered through feeding apparatus.
That said, breastmilk in any form (raw human milk, pasteurized human milk, individual donor milk or pooled breastmilk…) will always be superior to “formula” or artificial baby milk which is always at risk for contamination: on the production site (check out here) and through preparation (follow WHO Guidelines for the safe preparation, storage and handling of powdered infant formula)
Breastfeeding and epigenetics
Risks of artificial feeding
The risks of formula feeding are essentially depriving the child of the numerous biodynamic ingredients provided by breast milk. For information on the benefits of breastfeeding, see The Lancet Breastfeeding Series 2016. In terms of regulating short and long-term health, keep in mind that “Industrial milks contain almost none of the immunomodulatory components of human milk, and they do not provide a dynamic, personalised nutritional intake.” See above, Ames SR et al. 2023 https://pubmed.ncbi.nlm.nih.gov/37055920/
These risks are known for a long time. The following document by Dr Jack Newman lists research items about the negative impact of articifial feeding as of 1998.
